The advent of digital health has markedly influenced the transformation from laboratory research to clinical practice in diagnostics. This evolution encompasses the collection, storage, retrieval, transmission, and utilization of data, information, and knowledge to support healthcare.
Advancements in Diagnostic Healthcare
Electronic Signals at the Forefront
Digital health, embodying electronic signals, plays a pivotal role in enhancing the accuracy and timeliness of information transfer, crucial for effective decision-making in diagnostics.
In the field of pathology and medical imaging, the impact of digital health is profound. The integration of linked and interoperable electronic systems across various healthcare settings is essential for the seamless flow of patient information.
These systems not only facilitate the diagnostic process but also enable the monitoring of patient outcomes and hospital admissions, offering a more comprehensive picture of healthcare quality.
Moreover, digital health has been instrumental in standardizing diagnostic practices, as seen in initiatives like the Sensible Test Ordering Practice (STOP).
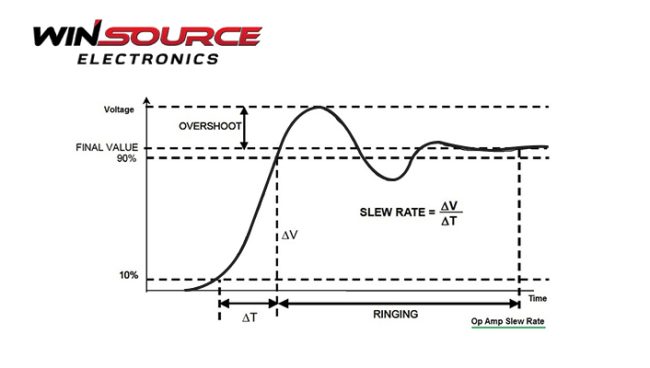
STOP utilizes a traffic-light system to guide the ordering of diagnostic tests based on the clinician’s seniority, thereby ensuring consistency and rationality in test ordering practices. It is particularly vital in acute care settings, where the slew rate of patient intake and complexity of cases demand efficient and accurate diagnostic processes.
However, the integration of digital health into clinical practice is not without challenges. The effectiveness of electronic decision support systems in reducing misdiagnosis is still under validation, with their impact on patient outcomes not being conclusively proven.
Furthermore, the introduction of such systems in clinical settings often faces hurdles due to limited pilot testing and a lack of understanding of their impact on existing workflows.
Diagnostic Errors in Healthcare
Prevalence and Impact of Diagnostic Errors
Diagnostic errors significantly impact patient safety in healthcare, contributing to approximately 10% of patient deaths and 6-17% of hospital adverse events.
In Australia, these errors are implicated in half of the medical negligence claims involving general practitioners.
Factors leading to diagnostic errors include fragmented care pathways, multiple specialist involvements, communication gaps among clinicians and patients, and inadequate infrastructure supporting the diagnostic process.
In acute care, laboratory testing is often underutilized (45%) or overutilized (21%).
Digital Health in Quality Improvement
Digital health provides key outcome-based measures of diagnostic utilization, such as patient outcomes or hospital admissions, essential for evaluating interventions like electronic decision support systems. These systems aim to address diagnostic errors by improving follow-up of test results and managing care transitions effectively.
Test Result Management and Follow-Up
The Significance of Test Result Follow-Up
Test result management and follow-up in healthcare are crucial components that can significantly impact patient safety and care quality. Deficits in the follow-up of test results are a major source of diagnostic error.
Studies indicate that a significant proportion of patients are discharged from hospitals with at least one test result pending. These lapses can lead to medication errors, medical errors in completing diagnostic workups, and loss of essential patient information, particularly during care transitions between healthcare settings.
Innovations in Pathology and Medical Imaging
The evolution of digital health has substantially influenced pathology and medical imaging services, enhancing the reliability and accuracy of diagnostic results.
Digital health tools, such as whole slide imaging (WSI) in digital pathology, have transformed diagnostic evaluations, enabling pathologists to view and navigate digitized slides akin to traditional glass slides.
The technology has been widely adopted for clinical, educational, and research purposes, underscoring the importance of integrating digital health systems into clinical practice for improved patient outcomes.
Patient Engagement Through Diagnostic Informatics
Empowering Patients with Decision-Making Tools
Diagnostic informatics and digital health stewardship have significantly shifted the landscape of patient engagement in healthcare. These advancements enable patients to participate actively in their own care decisions.
Patient decision aids, encompassing a range of digital tools, are pivotal in this transformation. These aids empower patients to clarify and communicate their subjective values and preferences regarding medical choices.
Patients and healthcare professionals can collaboratively determine the most appropriate medical interventions by understanding these preferences.
Digital Health Transforming Patient Care
The ReMiND project in India and AccuHealth in Chile demonstrate how digital health tools can significantly improve healthcare outcomes.
In India, a basic mobile health (mHealth) application has boosted the performance of community health workers, leading to marked improvements in maternal and infant health outcomes in rural communities.
In Chile, remote monitoring, artificial intelligence, behavioral nudging, and comprehensive support have significantly enhanced the quality of life for individuals with chronic conditions.
Challenges and Limitations in Electronic Decision Support Systems
Implementation Hurdles in Clinical Settings
Implementing electronic decision support systems (CDSS) in clinical environments presents unique challenges.
One case study of the CV Wizard, an electronic health record embedded CDSS, found its use in only 19.8% of eligible clinical encounters in community health centers. The low uptake shows the complexities of integrating CDSS into diverse healthcare environments.
Factors such as varying protocols, alert fatigue, and time constraints among healthcare staff contribute to reduced effectiveness. The study highlights the need to tailor CDSS to specific clinical contexts and recipient characteristics, ensuring that these systems do not overly burden healthcare professionals.
Clinical Decision Support Systems (CDSS): Usage and Adoption
CDSSs are designed to assist with patient risk prediction, prescribing safety, and diagnosis. Despite their potential benefits, there is evidence of low uptake and dissatisfaction among General Practitioners.
For successful adoption, developers need to focus on creating systems that align with clinical workflows, provide clear clinical pathways, and offer necessary training for practice staff.
AI in Electrocardiogram (ECG) Interpretation: Progress and Challenges
The integration of AI in ECG interpretation, particularly through deep-learning convolutional neural networks, marks significant progress in cardiovascular diagnostics.
This technology enables human-like interpretation of ECG, identifying complex patterns and signals. However, challenges persist, including ensuring data quality control, validating external applicability, and demonstrating improved patient outcomes.
AI–ECG has shown promising results in detecting various cardiac conditions and patient phenotypes but still requires human oversight for accuracy and to avoid systematic errors.
As you navigate the dynamic landscape of electronics in diagnostics, remember the pivotal role of quality components. For your next project, choose WIN SOURCE, where you’ll find a vast selection of authentic and reliable electronic components.
Act now to ensure your diagnostics technology stays ahead in efficiency and accuracy.

COMMENTS